Some basic biology
To better understand how to get pregnant, you need to know a bit of biology to optimise your chances.
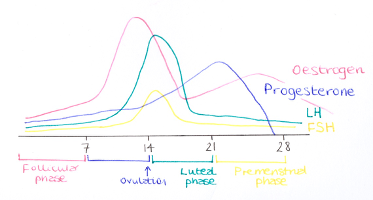
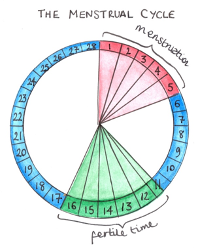
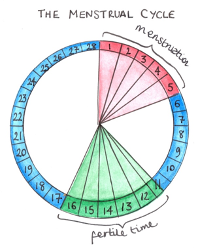
Menstrual cycle
- It’s important to understand this as you are most likely to get pregnant if you have sex within a day or so of ovulation. Ovulation is where an egg is released from the ovary.
- Day 1 of your menstrual cycle is counted from the first day of your period.
- Ovulation tends to occur 14 days before your period begins.
- If you have a 28-day menstrual cycle, your day of ovulation will be around day 14.
- If you have a longer cycle, your ovulation day might be later and if you have a shorter cycle, it might be earlier.
- Someone with a 32 day cycle is likely to ovulate around day 18 and someone with a 24-day cycle is likely to ovulate around day 10.
Lifespan of an egg
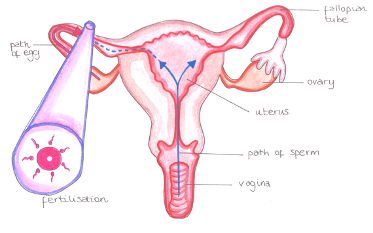
Once you ovulate, an egg lives for about 12-24 hours after it is released. The egg needs to be fertilised by a sperm within this time for a pregnancy to be achieved.
Lifespan of a sperm
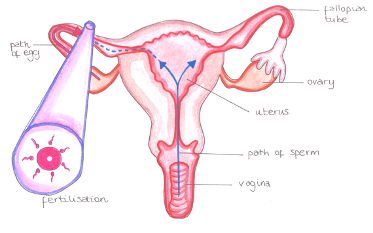
Sperm can live for up to 7 days inside a woman’s body. If you have had sex in the days before you ovulate, the sperm will have had time to travel up the womb to the fallopian tubes to ‘wait’ for the egg.
Timing and frequency of intercourse
Considering the biology discussed above, it is therefore important to have sex every 2 to 3 days throughout the month to give you the best chance. You do not need to limit sex to just the time around ovulation. For most people, sex is a pleasurable thing and you should continue to have it for this reason as before! Keeping sex enjoyable will help you limit stress around conceiving and help you to concentrate on your relationship.
Positions for sex
The position in which you have sex doesn’t make a different to conception as long as ejaculation occurs within the vagina. Once this has occurred, the sperm will swim up through the cervix and into the womb towards the fallopian tubes and meet an egg if it is there.
People talk about raising legs after sex to optimise conception. There is no evidence for this as the route to the fallopian tube is not a straight line!
Woman’s monthly cycle
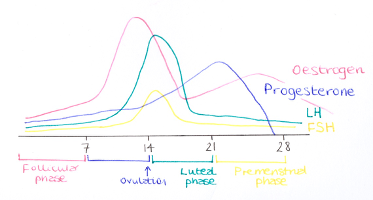
At the same time as the egg is released at ovulation, the lining of the womb begins to thicken and the mucus in the cervix (neck of the womb) becomes thinner so sperm can travel through it more easily.
Some women find having an awareness of their discharge helps them to time intercourse. Fertile discharge is thin, clear and more slippery. Some describe it looking a bit like egg white. Noticing a change in discharge can signal that ovulation is approaching.
Some women like to be aware of the timing of their ovulation. Your temperature rises by about 0.20C when ovulation has occurred. It is best to check your temperature each morning when you wake up. It only indicates that you have ovulated and not when it is the fertile part of your cycle.

Some women like buying an over the counter ovulation test kit. They work by detecting a hormone in your urine that increases just prior to ovulation. The simplest test kits check for luteinising hormone (LH) which peaks 24-36 hours before ovulation. This therefore helps to flag your best two days to attempt conception. It is best to have idea of your cycle length to know when to start testing in the month. Ovulation kits can also be helpful for those with irregular cycles but you will obviously need more strips.
If an egg is fertilised by a sperm, it then needs to implant in the thickened womb lining. If an egg is not fertilised, it will pass out of the body during the next period. Eggs are very small and not visible to the naked eye.
Stopping contraception
If you have been taking a form of hormonal contraception for a while, you might not know what your regular menstrual cycle is like. This includes the pill, patches, injections and hormonal coil. It might take a month or two after stopping for your own hormones to regulate.
Hormonal contraception does not cause infertility, but it can cover up conditions that are linked to infertility because of a lack of periods. This includes conditions like endometriosis and PCOS (polycystic ovarian syndrome).
Specifics about stopping contraception:
- The Pill (combined oral contraceptive)
- Finish the current packet.
- You can time your pregnancy better if you wait for first period after stopping (not the initial withdrawal bleed). This can take 4-6 weeks after finishing a packet.
- You won’t harm the baby if you get pregnant sooner.
- Mini-pill (progesterone only pill)
- Stop at any time in the packet.
- Can time pregnancy better if you wait for first period after stopping. This can take 4-6 weeks after finishing a packet.
- You won’t harm the baby if you get pregnant sooner.
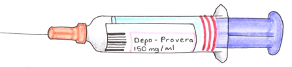
- Contraceptive injections (e.g. Depo – provera)
- Don’t renew injection when it is due.
- Can time pregnancy better if you wait for first period after stopping. This can a few months from the last injection.
- Progesterone implants (e.g. implanon)
- Make appointment with your doctor to have this removed.
- Can time pregnancy better if you wait for first period after stopping. This can a few weeks from removal.
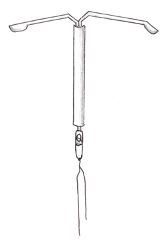
- Intrauterine device (e.g. copper coil or mirena coil)
- Make appointment with your doctor to have this removed.
- Can time pregnancy better if you wait for first period after stopping. This can a few weeks from removal of a hormonal coil like the mirena.
Confirming pregnancy
If you miss a period, you might be pregnant. Sometimes, cycles that have always been regular might fluctuate when trying to conceive.
You can carry out a home pregnancy test from the first day of a missed period.

If you aren’t sure when your last period was, you can carry out a pregnancy test from a minimum of 21 days after unprotected intercourse.
Some pregnancy tests are very sensitive, and you can carry one out 8 days after conception which is before your period would be seen.
You can buy pregnant tests in any pharmacy, supermarket or online.
Pregnancy tests detect a hormone called human chorionic gonaotrophin (hCG) which starts to be produced 6 days after fertilisation.
All pregnancy tests are slightly different so it’s best to follow the instructions inside the kit.
A positive test is almost always current. A negative result can on occasion be incorrect. If you still do not start your period, consider repeating the test a day or two later.
If you have irregular or long menstrual cycles, you might develop some of the symptoms of early pregnancy and this would prompt you to do a pregnancy test. These include:
- Extreme tiredness
- Nausea
- Metallic taste in mouth
- Sensitivity to smells
- Breast tenderness
- Need to wee more frequently
Once pregnant…
You can self-refer for antenatal care. This can be done through hospital websites.
Your first official scan on the NHS will be your dating scan at 11-13 weeks.
If you develop any bleeding or pain before this, an early pregnancy scan might be indicated. You can contact your GP or local early pregnancy unit within the NHS Hospital.
If you wish to have an early pregnancy scan, this can be arranged privately. This is best carried out from 6 weeks. Pregnancy is dated from the first day of your period. So 6 weeks will usually be 2 weeks after a missed period. Waiting until this time allows for ultrasound to be more accurate at detecting the site and size of the developing pregnancy and provide more reassurance.
Active measures for women to help achieve a healthy pregnancy
Alcohol
- The Chief Medical Officers for the UK advise that if you are planning to get pregnant, the safest approach is to avoid drinking alcohol.
- Alcohol can pass from your blood through the placenta and to your baby.
- Drinking alcohol in pregnancy, especially in the first 3 months can affect your baby after they’re born.
- The risks are greater the more you drink.
- As you don’t know how long it might take you to get pregnant, it is sensible to simply avoid heavy drinking when trying to conceive.
- If you find out you are pregnant after having drunk in early pregnancy, try not to worry as the risks to baby are likely to be low.
Smoking
- Smoking affects fertility in women and men.
- Smoking has been shown to damage the DNA of your baby.
- Protecting yourself and your baby from tobacco smoke it one of the best things you can do.
- Stopping smoking will immediately reduce your risk of pregnancy and birth complications.
- If you need support with stopping smoking for you and/or your partner, the NHS has a Smokefree helpline open 9am to 8pm Monday to Friday.
Drugs
- Using illegal drugs such as cannabis, cocaine and other drugs have been associated with fertility problems.
- Illegal drugs are associated with several significant pregnancy problems including premature birth and stillbirth.
Exercise
- Women who do regular, moderate exercise get quicker than women who don’t exercise regularly.
- Anything that makes your heart rate increase or breathing faster is good. Going for a brisk walk is moderate activity.
- If you regularly do vigorous or intense exercise but are used to this and are having regular periods, you can continue this.
- If you are missing period and do intense vigorous exercise and are struggling to get pregnant, it might be worth bringing your activity level down to moderate. This tends to only affect elite athletes as the intense physical activity might be altering hormone levels.

Nutrition
- A healthy diet is an important part of a healthy lifestyle at any time.
- Try to maintain a healthy weight and aim for a BMI before conception of 18.5 to 24.9.
Click here to calculate your BMI:
https://www.nhs.uk/live-well/healthy-weight/
- It is important to get a good balance of food groups.
- Foods to avoid when trying to get pregnant or when pregnant:
- Mould ripened cheese with a white coating e.g. brie or goats cheese (unless piping hot), Soft blue cheeses and any unpasteurised cheeses – associated with an infection called listeriosis.
- Raw or undercooked meat and cured meats – associated with an infection called toxoplasmosis.
- Liver and liver products – high levels of vitamin A.
- Raw or partially cooked eggs that are not British Lion stamped – associated with an infection called Salmonella.
- Limit oily fish (salmon, trout, mackerel or herring) to twice a week as they may contain pollutants.
- Limit tuna to 2 tuna steaks or 4 medium sized cans because they contain mercury.
- Avoid shellfish as they can contain bacteria, viruses or toxins.
Caffeine
- You can have caffeine when trying to conceive but try to reduce your consumption to 200mg a day.
- 100mg in a mug of instant coffee.
- 140mg in a mug of filter coffee.
- 75mg in a mug of tea (green tea can have the same amount of caffeine as regular tea).
- 40mg in a can of cola.
- 80mg in a 250ml can of energy drink.
- less than 25mg in a 50g bar of plain dark chocolate.
- less than 10mg in a 50g bar of plain milk chocolate.
- Some research has shown an increased risk of miscarriage if having too much caffeine.
Folic Acid
- Folic acid helps to protect a baby from getting a neural tube defect.
- It is best to start taking this before you get pregnant to boost your levels.
- Most women need to take 400mcg folic acid daily which can be purchased over the counter in any pharmacy and most supermarkets.
- Some women need a higher dose of 5mg if they have diabetes, epilepsy or a previous pregnancy affected by a neural tube defect. This dose will need prescribing by a doctor.
Vitamin D
- All women are advised to take 10 micrograms of vitamin D daily throughout pregnancy and ideally pre-conception.
- You can buy this over the counter on its own or in combination with folic acid.
Underlying medical conditions
- If you have any chronic health issues like diabetes, high blood pressure, high cholesterol, kidney disease, asthma, mental health conditions or epilepsy, it is important to involve your GP or specialist before attempting conception.
- Seeing a specialist will allow for stopping any medications that are not safe in pregnancy and optimising your health.
- Also in general – if you are due or almost due a cervical smear test, it is good to have this done pre- conception. This is especially important if you have previously had abnormal cells detected.
- If you have not been vaccinated for Measles, Mumps and Rubella (MMR) or you are unsure, it is useful to address this before conception.
- If you have not had a recent sexual health screen for infections like chlamydia or HIV and are planning to stop barrier contraception (condoms/femidoms), it is sensible to consider this first. Some sexually transmitted infections can impact on fertility and pregnancy.
Active measures for men to help achieve a healthy pregnancy
All too often, the focus on fertility conversations revolve around the women. However, there are plenty of things men can do to help too!
Alcohol
- The recommended limit on alcohol is 14 units of alcohol per week.
- Excessive alcohol can reduce a man’s interest in sex and reduce testosterone levels.
- Alcohol can also affect the quality and quantity of sperm.
- Cutting down alcohol to no more than 3-4 units a day should be the aim.
- Supporting your partner with cutting down alcohol consumption can be very helpful as women are advised to avoid alcohol when trying to conceive.
- If you have been drinking more than the recommended amount, the good news is that the changes are all reversible as men are continually producing new sperm.
Smoking
- Smoking can reduce the quality and quantity of sperm. It can also reduce the sperm’s ability to swim (motility).
- Smoking can also be associated with male sexual impotence.
- Stopping smoking can reverse the damage.
- If you need support with stopping smoking for you and/or your partner, the NHS has a Smokefree helpline open 9am to 8pm Monday to Friday.
Drugs
- Using illegal drugs such as cannabis, cocaine and other drugs have been associated with fertility problems.
- Cannabis can lower testosterone and effect the quality of sperm.
- Cocaine can reduce the enjoyment of sex and cause difficulties with erections and sperm production.

Stress
- Stress can affect your relationship and reduce your sex drive. This might impact on the frequency you are able to have sex.
- Severe and ongoing stress can limit sperm production.
- For some people, trying to conceive a baby can be stressful. Try to take the time to relax.
Sperm temperature
- The testicles (balls) are outside of the body as sperm quality is best when they are kept slightly cooler than body temperature.
- Try to avoid overheating your testicles e.g. warm laptop on your lap, hot saunas, hot baths, tight lycra for long periods of time.
Nutrition
- Diets high in processed meat, alcohol, caffeine, red meat, saturated fatty acids and trans fats were linked to low quality semen.
- Diets rich in fruits, vegetables, whole grains, fish were linked to better semen quality.
- Eating a portion of walnuts a day has been shown to have a help sperm motility (ability to swim).
- Being obese (having a BMI above 30) has been associated with a reduction in sperm quality and quantity.
- High levels of caffeine have been shown to increase the rates of miscarriage. Try to limit our caffeine to 200mg a day which is roughly 2 mugs of instant coffee or 1 mug of filter coffee.

When to seek medical help
The reality: Around 1 in 7 couples will have difficulties getting pregnant.
The general advice is to see your doctor if you have not conceived after one year of regular unprotected intercourse.
There are certain situations where it is worth seeing your doctor a bit earlier:
- Maternal age – if you are over 36, it is worthwhile having some baseline fertility investigations a little sooner. It is recommended to consider fertility checks after 6 months of attempting pregnancy once over the age of 35. Fertility does decrease with maternal age. Whilst many women do decide to have babies later in life and do so successfully, some might need medical help. After the age of 35, a woman’s fertility decreases as the number and quality of eggs reduces. In women ages 40-42 who have not conceived after 2 years of regular unprotected intercourse, or 12 cycles of artificial insemination (where 6 or more are by intrauterine insemination), the NHS offers 1 full cycle of IVF, providing certain criteria are met.
- Paternal age – this is less problematic than in women. However, increasing paternal age is associated with less interest in sex, poorer quality sperm and lower levels of sex hormones.
- Irregular or no periods – without a regular menstrual cycle, it will be very difficult to know if you are ovulating and how-to time intercourse. Baseline hormonal tests can help to determine these things. It would be advised to see a doctor within a couple of months of starting to get pregnant if this is your situation.
- Known fertility issue – is you are known to have endometriosis or polycystic ovarian syndrome; it is worth an early review by a gynaecologist. These conditions are associated with reduced fertility. Many women with these conditions do get pregnant with little or no fertility treatment. Baseline blood tests and an ultrasound can help to establish the likelihood of this impacting on your fertility.
- Partner has a known fertility issue – If you are aware of having a low sperm count or had previous testicular or genital surgery, it might be worth having an early semen analysis to check the quantity and quality of sperm.
- Medical issues – if you are known to have a health condition that might impact on your fertility then it might be worth an early gynaecological assessment. This might include previous cancer treatment, endocrine problems like thyroid dysfunction or pituitary problems. If you take medication for a health condition that might not be safe in pregnancy, you might also want a medical consultation early.
- Difficulties having intercourse – this can be especially problematic when trying to conceive. Struggling with painful intercourse, vaginismus, reduced libido and erectile dysfunction can all make regular sex and conception difficult. Seeing a specialist might help with advice and improve your chances of getting pregnant.
- Anxiety- for some couples, the pressure of getting pregnant and the disappointment of being unsuccessful each month can be very upsetting. Stress can challenge a relationship. Earlier investigations in these situations and some general guidance can be helpful.
- Previous or recent sexually transmitted infection – if you or your partner have had previous chlamydia, gonorrhoea, hepatitis, HIV or syphilis, it is worth an early gynaecological consultation to plan your pregnancy safely. History of female chlamydia or gonorrhoea is associated with fallopian tube dysfunction so an earlier assessment of this would be recommended.
Baseline fertility tests
The specifics of the different tests available can be very confusing. The terminology surrounding fertility treatment is also difficult. Below we will discuss the various tests that are normally carried out as part of ‘routine’ fertility checks. Tests will be offered based on your own personal situation.
Tests for men
- There is generally just one type of test for man. This is a semen analysis. You will be asked to produce a semen sample and it will be assessed for the quality and quantity of sperm. The sample is produced by masturbation with a 3-4-day abstinence period before. If the result is abnormal, you might be asked to repeat it at a 6-week interval as sperm production is continually cycling and it might be normal on the next occasion.

Tests for women
- Hormonal blood tests – these will help to ensure that your ovaries are functioning, check you are ovulating, rule out thyroid dysfunction and other hormonal imbalances.
- Pelvic ultrasound – This is normally an internal (transvaginal) scan. This can ensure you have normal appearances of your ovaries and uterus (womb). It can be used to assess your womb lining and, in some instances, your follicles. Simple things like fibroids, polyps and ovarian cysts might be detected and by dealing with them, this might improve your fertility. You will be asked to have an empty bladder for this test.
- Anti-Mullerian Hormone (AMH) – this is a blood test that can help to find out what your ovarian reserve is. Put simply, it is a marker of how well your ovaries are working.
- HyCoSy – this is short for a Hysterosalpingo Contrast Songography. Essentially it is a specialised internal pelvic ultrasound to visualise whether your fallopian tubes by passing a dye through them. You need at least one functioning fallopian tube to get pregnant. You will be asked to have an empty bladder for this test.
- Smear test – this is unlikely to reveal an underlying fertility issue but is well worth ensuring your smear test is up to date with the screening programme.
Fertility treatment
Fertility treatment will depend on the results of your tests.
There are essentially three main types of treatment:
- Drugs to improve ovulation – this can be provided outside of a bespoke fertility centre. Problems with ovulation are the most common cause of infertility. The drugs can help with this include clomifene, letrozole, metformin and gonadotrophins. Choice of drug will depend on your own underlying reproductive and general health.
- Surgery if there are blockages in the fallopian tubes or signs of endometriosis. This is normally keyhole (laparoscopic) surgery.
- Assisted conception – this includes intra-uterine insemination (IUI) and in-vitro fertilisation (IVF). These treatments will be offered at a dedicated fertility unit.
COVID-19 and pregnancy
The international pandemic COVID-19 has had repercussions across healthcare. It has some specific implications on conception and pregnancy.
For the latest guidance on this, it is best to refer to the Royal College of Obstetricians and Gynaecologists (RCOG) guidance; https://www.rcog.org.uk/globalassets/documents/guidelines/2020-04-27-occupational–health–advice–for–employers-and–pregnant-women.pdf
https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-pregnancy/covid-19-virus-infection-and-pregnancy/
As of early June 2020, the most relevant key points are as follows:
- It is an evolving situation and the effects of this disease in pregnancy are not fully understood yet.
- Pregnant women do not appear more likely to contract the infection despite changes in the immune system during pregnancy.
- There is no current evidence that pregnancy women are more likely to become severely unwell.
- Most pregnant women will experience only mild or moderate cold/flu-like symptoms.
- There is currently no data to suggest an increased risk of miscarriage in relation to COVID-19.
- Pregnancy care has not altered unless you or a household member develop symptoms in which case a routine appointment or scan might be modified.
- Women from a BAME (black and minority ethnic) group are at higher risk of complications from COVID-19.
- If you are self-isolating, stay hydrated and mobile as COVID-19 is associated with development of deep vein thrombosis (DVT) and pulmonary embolism (PE). Pregnancy also increases your risk of this. If you are receiving fertility treatment or become pregnant, a risk assessment will be carried out to determine if you need any treatment to reduce your risk of clot formation.
- As per government guidance, it is important to practice social distancing, wash your hands regularly and wear a face covering on public transport.
- Pregnant women are placed in the UK government’s vulnerable group and therefore advised to stay at home and work from home, when possible.
- It is important to be aware that the pandemic might impact on who can attend appointments with you. Please check in advance to avoid disappointment. This is to limit the potential spread of infection.
Author Dr Irene Gafson is an Obstetrician and Gynaecologist with an interest in medical and patient education. She works as a post-CCT fellow at the Whittington hospital and a senior teaching fellow at UCL medical school. Illustrations by Dr Eleanor Fleming.
DISCLAIMER
This article is for information only and should not be used for the diagnosis or treatment of medical conditions. Essential Parent has used all reasonable care in compiling the information from leading experts and institutions but makes no warranty as to its accuracy. Consult a doctor or other health care professional for diagnosis and treatment of medical conditions. For details
click here.

![]()